Published: October 2025
This guide is written for anyone who suddenly lost vision or developed sudden blur in one eye and was medically reviewed by an eye doctor. Sudden vision changes can be an emergency.
You wake up and one eye is blurry. Or you’re fine all day, and suddenly the vision in one eye looks cloudy, gray, or like someone put a smudge in the middle. It doesn’t always hurt. That makes people think, “Maybe I’ll wait and see if it clears.” You should not wait. Sudden blurry vision in one eye (or sudden vision loss in one eye) can be a sign of retinal detachment, an “eye stroke,” severe eye infection, dangerously high eye pressure, or inflammation of the optic nerve. Some of these can cause permanent vision damage within hours if you delay care.:contentReference[oaicite:0]{index=0}
This article explains why sudden blur in one eye is different from “I probably just need new glasses,” which symptoms mean same-day emergency care, and what you should tell the eye doctor when you get there. You’ll also learn when online help is useful — and when it is absolutely not enough.
Why Sudden Blurry Vision in One Eye Can Be Dangerous
Gradual blur in both eyes over months often means something simple like you need new glasses or you’re dealing with dry eye or screen strain. Sudden blur in one eye is different. Doctors treat it like “something changed inside the eye or along the vision pathway right now.” That could mean a torn retina, a blocked blood vessel, swelling under the macula (the center of sight), very high eye pressure, or inflammation of the optic nerve. All of those can seriously threaten sight.:contentReference[oaicite:1]{index=1}
Here are the most urgent causes your eye doctor will think about first.
Retinal Detachment or Retinal Tear
The retina is the light-sensing tissue in the back of the eye. If the retina pulls away (detaches), the part that is lifted up stops working. You lose vision in that area — it can look shadowy, gray, or like a “curtain” coming across your sight. A retinal detachment or a severe retinal tear is an emergency. The longer the retina stays detached, the higher the risk of permanent vision loss.:contentReference[oaicite:2]{index=2}
Common warning signs include:
- A sudden burst of new floaters (dots, strings, cobwebs) in one eye.
- Flashes of light that look like lightning or camera flashes, especially in the side vision or in the dark.
- A dark shadow, veil, or curtain moving over part of your vision from the side or top.:contentReference[oaicite:3]{index=3}
Floaters alone are common with normal aging of the eye’s gel (called posterior vitreous detachment), and most of the time that is not dangerous. But a sudden shower of new floaters plus flashes plus “part of my vision just went dark” can mean a tear that is pulling on the retina. That must be seen the same day by an eye specialist (retina specialist) so it can be sealed with laser or treated surgically before vision is lost permanently.:contentReference[oaicite:4]{index=4}
Central Retinal Artery Occlusion (“Eye Stroke”)
If you suddenly lose most or all vision in one eye — and it’s painless — doctors worry about central retinal artery occlusion (CRAO). CRAO is often described as a stroke of the retina. A blood vessel that feeds the retina becomes blocked, so the retina is suddenly starved of oxygen. Vision can drop in seconds. This is considered a form of acute ischemic stroke, and you need emergency medical attention right away.:contentReference[oaicite:5]{index=5}
People describe it like:
- “I looked up and my right eye just went dim.”
- “There’s a gray fog covering everything in one eye.”
- “It’s like someone pulled down a shade over that eye.”
Even though the term “eye stroke” sounds dramatic, it’s accurate. CRAO is treated as a stroke emergency because it not only threatens sight, it is also linked with higher risk of stroke in the brain and heart disease. Some hospitals now have rapid-response protocols to evaluate and treat CRAO urgently to try to protect vision, but timing matters. Hours matter. If one eye suddenly goes dark, you should be evaluated as an emergency, not told to “come back next week.”:contentReference[oaicite:6]{index=6}
Acute Angle-Closure Glaucoma (Dangerously High Eye Pressure)
Glaucoma is usually thought of as a slow disease with no symptoms at first. But there is a fast, emergency version called acute angle-closure glaucoma. In this condition, the pressure inside the eye spikes very quickly. That pressure can crush the optic nerve — the cable that carries vision to your brain. Permanent vision loss can happen very fast if it is not treated.:contentReference[oaicite:7]{index=7}
Symptoms often include:
- Severe eye pain, usually in one eye.
- Sudden blurry or hazy vision in that eye.
- Halos or rainbow rings around lights.
- Red eye.
- Headache, nausea, or even vomiting.:contentReference[oaicite:8]{index=8}
This is not “eye strain.” This is an emergency. The eye needs its pressure lowered quickly, sometimes with special drops and medications, sometimes with a laser procedure to create a new fluid pathway. If you notice sudden one-eye blur plus severe pain, halos, and nausea, you should seek urgent in-person care immediately.
Severe Corneal Infection or Ulcer (Especially in Contact Lens Wearers)
The cornea is the clear front surface of the eye. If bacteria get into it — for example, from sleeping in contact lenses, swimming in lenses, wearing lenses too long, or using lenses that don’t fit — you can develop a corneal ulcer. A corneal ulcer can scar in hours and permanently affect vision.:contentReference[oaicite:9]{index=9}
Warning signs of a serious corneal infection include:
- A very red, very irritated eye (usually one eye).
- Sharp pain or the feeling “there is glass in my eye.”
- Trouble keeping the eye open because light hurts.
- Sudden blurry vision in that eye.
- Sometimes, a white spot on the cornea.:contentReference[oaicite:10]{index=10}
This is urgent. You should stop wearing contact lenses immediately and be seen the same day. Do not rinse the lens and put it back in. Do not use leftover antibiotic drops from a family member. Corneal ulcers need the correct prescription drops, often started right away, to prevent permanent scarring and permanent vision loss.:contentReference[oaicite:11]{index=11}
Optic Neuritis (Optic Nerve Inflammation)
The optic nerve is the cable that carries vision signals to your brain. When it becomes inflamed, that’s called optic neuritis. Optic neuritis can cause rapid vision loss or a large blurry “smudge” in one eye over hours to days. People often say vision looks dimmer or washed out in that eye. A classic clue is that it hurts when you move the eye.:contentReference[oaicite:12]{index=12}
Optic neuritis needs urgent medical attention. It can be linked with inflammation in the body or brain, and sometimes with neurologic conditions such as multiple sclerosis. Early evaluation can help protect vision and guide treatment, which may include steroids or other therapy depending on the cause. Doctors generally tell patients: if you have sudden vision loss, get examined right away.:contentReference[oaicite:13]{index=13}
When Sudden Blur Is Less Dangerous
Not every episode of one-eye blur is permanent damage. For example, some people get a temporary visual change from migraine aura: flickering zigzags, shimmering shapes, or a patch of vision that goes gray and then returns in 20–30 minutes. That can happen even without a headache. Migraine aura can be scary, but it usually comes and goes, and full vision often returns quickly. Still, you should not assume it’s “just migraine” the first time it happens. A first-ever sudden vision loss still needs urgent medical evaluation to rule out retinal or vascular causes.:contentReference[oaicite:14]{index=14}
Dry eye can also blur vision, but that blur usually clears when you blink or use artificial tears and tends to affect both eyes, not one eye only. Dry eye does not cause a dark curtain, sudden missing vision, severe pain, halos with nausea, or a gray spot that stays in the center. If you have those symptoms, it is not “just dry eye.”
When You Need Same-Day Emergency Care
You should seek same-day in-person emergency eye care (or emergency department care that can reach an eye specialist) if you notice any of these:
- Sudden vision loss or a sudden dark/gray area in one eye.
- Sudden severe blur in one eye that was normal earlier today.
- A “curtain,” “veil,” or shadow coming across your vision.:contentReference[oaicite:15]{index=15}
- New flashes of light plus many new floaters.
- A painful, very red eye with halos/rainbows around lights, nausea, vomiting, or a bad headache.:contentReference[oaicite:16]{index=16}
- A white spot on your cornea and sudden blur, especially if you wear contact lenses.:contentReference[oaicite:17]{index=17}
If you have any of these, do not drive yourself unless your other eye is normal and safe to see with. Get someone to take you in, or call for urgent medical help.
How to Talk to the Eye Doctor (What to Say Immediately)
When you arrive in urgent care or call the clinic, use simple, direct language. You can say:
- “My right eye suddenly went blurry about one hour ago. I can’t read with it.”
- “I see a dark curtain over the bottom half of my left eye.”
- “I have severe eye pain, nausea, and halos around lights in one eye.”
- “I wear contact lenses and now I have sharp pain and light hurts.”
Those phrases tell the provider this is urgent retina / cornea / optic nerve / high-pressure territory, not a routine “I think I need new glasses.” That helps you get seen faster.
Where Online Help Fits — and Where It Stops
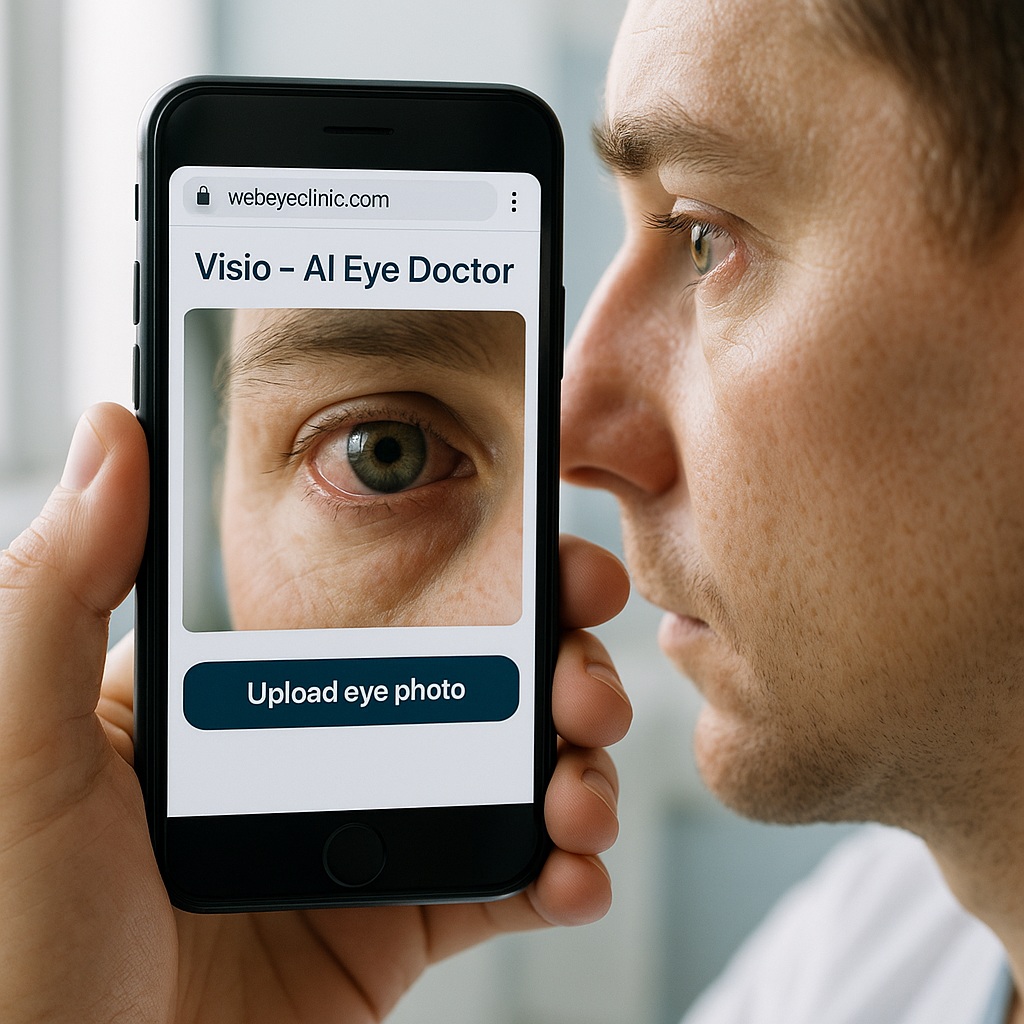
Online tools, including our own Ask the Eye Doctor service on WebEyeClinic, can help you describe exactly what you’re seeing and prepare you to speak to an in-person doctor without freezing or forgetting details. We can also help translate your symptoms into medical language, especially if English is not your first language. That can save time in the clinic and make you feel heard.
But there is a hard safety rule: sudden vision loss, a curtain over part of your vision, severe one-eye pain with halos and nausea, or a white spot and severe light sensitivity after contact lens wear are physical emergencies. No chatbot, website, or AI model — including ours — can examine your retina, measure your eye pressure, or start treatment for retinal detachment, eye stroke, acute glaucoma, or a corneal ulcer. Those need a real exam the same day.:contentReference[oaicite:18]{index=18}
If you’re unsure, start here:
Ask the Eye Doctor.
You can describe your symptoms, and we’ll help you phrase them clearly so you can tell an eye clinic, “This started today. I am losing vision. I need to be seen now.”
Bottom Line: Do Not “Wait and See” With Sudden One-Eye Blur
If you have sudden blurry vision in one eye, sudden vision loss in one eye, a curtain or shadow in your vision, flashes and new floaters, or a painful red eye with halos and nausea, treat it like an emergency. Retinal detachment, eye stroke (central retinal artery occlusion), acute angle-closure glaucoma, severe corneal infection, and optic neuritis can all threaten sight quickly. Fast treatment can protect vision. Waiting can cost vision permanently.:contentReference[oaicite:19]{index=19}
Medically reviewed by: SR, MD, Ophthalmologist (Retina Specialist).
Last updated: October 25, 2025.