Published: November 2025
This guide is written for patients who suddenly developed a red eye and want to know what to do first. Reviewed by the WebEyeClinic medical content team.
Waking up with a red eye can be scary, especially if you don’t know whether it’s just irritation or the start of something dangerous. The tricky part is that “red eye” is a symptom, not a diagnosis. It can be as simple as a bit of dust, allergy, or staring at screens for hours — or it can be an early sign of a corneal infection, uveitis, or even angle-closure glaucoma, which are emergencies. The good news is that you can make a safe first move at home: stop contact lenses, clean the eye, cool it, and watch for red-flag symptoms. This article will show you exactly what to do for a red eye, how to tell pink eye from other causes, and when you must call an eye doctor the same day.
What Is a Red Eye?
A red eye (also called eye redness or conjunctival injection) means the blood vessels on the surface of the eye have opened up or become irritated. This can happen in the conjunctiva (the thin transparent tissue covering the white of the eye), in the eyelids, or sometimes in the front of the eye (the cornea and anterior chamber) if there is deeper inflammation.
Common, usually mild causes include:
- Viral conjunctivitis (often starts in one eye and spreads to the other)
- Allergic conjunctivitis (red + itchy + watery, often both eyes)
- Dryness or screen fatigue (burning, gritty feeling)
- Contact lens overwear (red, irritated, maybe slightly painful)
- Subconjunctival hemorrhage (a bright red patch after coughing, straining, or rubbing)
More serious causes include:
- Keratitis / corneal ulcer (often in contact lens wearers, painful, light sensitive)
- Uveitis / iritis (pain, light hurts, blurry vision)
- Acute angle-closure glaucoma (very painful, halos, nausea)
- Orbital or eyelid infection (swelling, fever, eye won’t open)
This is why every red eye needs a quick “is this safe or not?” check.
What to Do for a Red Eye Right Now
In many mild situations, you can start care at home straight away. Here is the safest first-line plan:
- 1) Stop wearing contact lenses immediately. Lenses can trap germs and worsen redness. Keep them out until the eye is white again + 24 hours.
- 2) Rinse or lubricate the eye. Use preservative-free artificial tears 4–6 times a day. This soothes and flushes irritants.
- 3) Apply a cool compress if the eye is hot, itchy, or allergic. 5–10 minutes, clean cloth, not directly icy.
- 4) Wash hands often and don’t share towels if you suspect infection.
- 5) Rest the eye from screens, smoke, and makeup for the day.
This simple plan helps many viral, allergic, or irritative red eyes feel better in 24–48 hours. But this plan assumes you do not have severe pain, light sensitivity, vision changes, or injury. If you do, skip home care and go straight to the urgent section below.
A lot of people ask, “Should I start antibiotic drops right away?” The answer is usually no. Most red eyes are viral or allergic, and antibiotics don’t help those. Using the wrong drop on a corneal infection can even delay the correct treatment. Let an eye doctor decide.
Daily Protection Plan for a Red Eye
You can support healing over the next couple of days with a simple routine:
Why does this help? Because a red eye is often a surface inflammation. If you remove triggers (lenses, makeup, screens, dust) and keep the surface moist, the blood vessels can calm down faster.
Focus on:
- Artificial tears every 3–4 hours while awake
- Cool or warm compress 2–3 times/day (cool for allergy, warm for eyelid/stye)
- Lid hygiene if crusting: gentle baby-shampoo or lid-wipe cleaning along the lash line
- No lenses, no rubbing, no eye-whitening drops (those can rebound)
- UV-blocking sunglasses outdoors if eyes are light sensitive
If you are prone to allergy-red eyes, start an antihistamine/mast-cell stabilizer drop recommended by your eye doctor at the beginning of the season.
When Do You Actually Need Eye Drops from a Doctor?
Not every red eye needs a prescription. But some do. Your doctor may prescribe:
- Antibiotic drops for bacterial conjunctivitis (sticky, pus-like discharge, often one eye first)
- Antihistamine or anti-allergy drops for itchy, watery, seasonal red eyes
- Antiviral or steroid drops for certain viral/inflammatory conditions (these must be supervised)
Older advice was “any red eye → take an antibiotic.” Newer, safer practice is “red eye + no discharge + no pain → start with lubrication and observation, and only treat when we know the cause.” This protects you from overuse of antibiotics and from masking dangerous corneal problems.
Important safety note: never start someone else’s steroid eye drop for a red eye. Steroids can make herpes eye infections and some fungal/ulcer problems much worse.
Learn more:
Chat with an eye doctor online
and
Can I send a photo of my eye to a doctor?
Lifestyle Risks That Make Red Eye Worse
Sleeping in contact lenses or wearing them longer than the recommended hours is one of the fastest ways to turn a harmless red eye into a corneal infection. If lenses are part of your routine, build in “eyeglasses days.”
Rubbing your eyes when they are itchy from allergy or dryness can break tiny vessels and spread infection. Use cold compress and drops instead.
Not cleaning makeup / eyelid margins can clog the oil glands, making dry eye and redness more likely. Remove eye makeup fully at night.
Red-Eye Alarm Signs — See an Eye Doctor Today
Go to an eye doctor, urgent care, or emergency department the same day if you notice any of these:
- Red eye + moderate or severe pain
- Red eye + blurry or reduced vision
- Red eye + light sensitivity (you squint or can’t open the eye)
- Red eye in a contact lens wearer that does not improve within hours of removing lenses
- Red eye after trauma (metal, plant, chemical, elbow, cosmetics)
- Swelling of eyelids or face, fever, difficulty opening the eye
These can mean keratitis, uveitis, scleritis, cellulitis, or acute glaucoma. Home care is not enough for those.
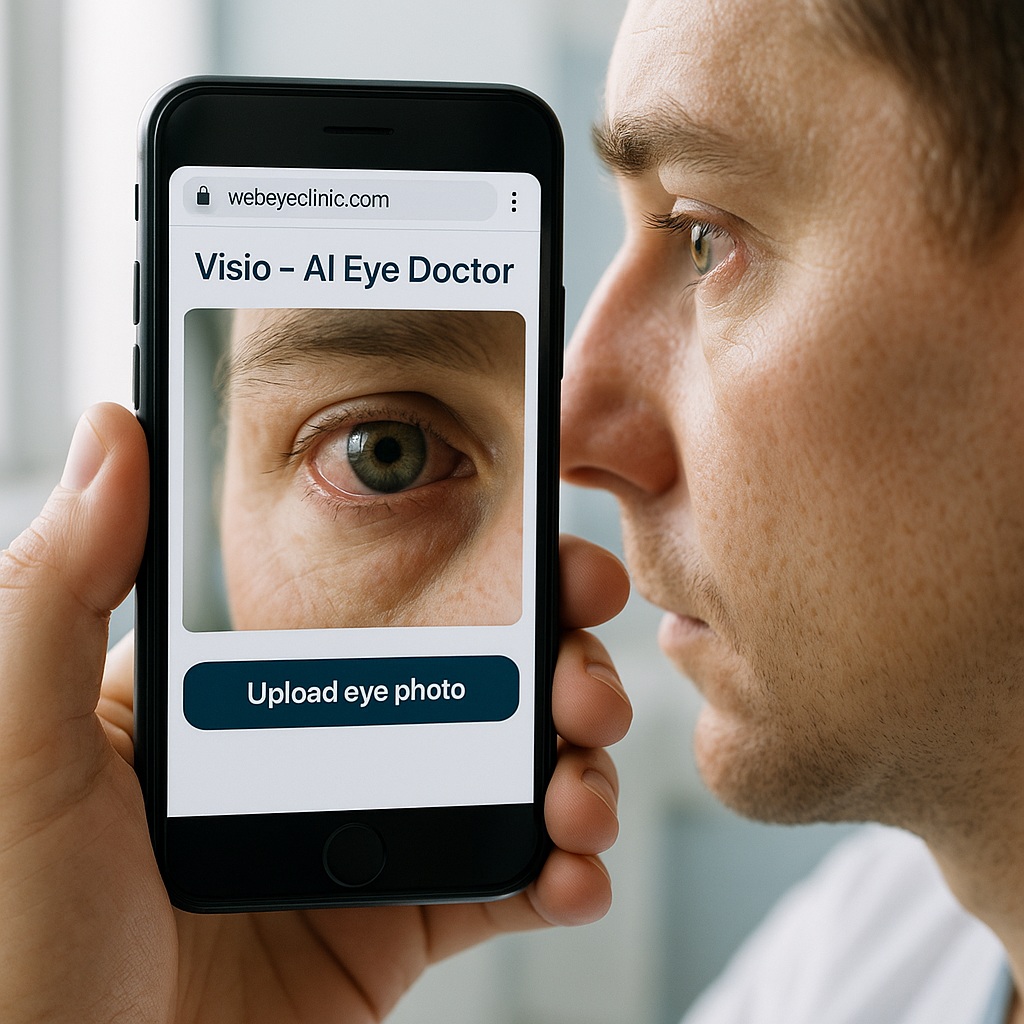
What’s New in Red-Eye Care
Teleophthalmology is making red-eye triage much faster. Many clinics, including WebEyeClinic, now let you upload a photo of your red eye and answer a short symptom form. AI (like Visio) can draft a likely cause and push urgent-looking cases to a human eye doctor first. That means people with painful, lens-related, or post-injury red eyes are seen first, while mild allergic/pink eye can be managed online.
There are also newer antihistamine/mast-cell stabilizer drops that work quickly for allergic red eye, and newer preservative-free artificial tears that are gentler for people who need drops often.
When You Should Call an Eye Doctor
Call if the red eye doesn’t improve in 48–72 hours with home care, comes back again and again, or happens together with headaches, halos, or vision changes. Call earlier if you have diabetes, autoimmune disease, or if the red eye is on an operated eye.
Even if your red eye gets better, still mention it at your next eye exam. Recurrent redness can point to dry eye disease, eyelid disease, or uncorrected vision strain.
Bottom Line: Treat the Cause, Watch the Warnings
You can safely start care for many red eyes at home: stop lenses, rinse with artificial tears, use a compress, and rest the eye. But if pain, light sensitivity, or blurred vision joins the redness — or if you wear contact lenses — act like it’s urgent and talk to an eye doctor the same day. Online photo uploads make that easier than ever.
Reviewed by: WebEyeClinic medical content team.
Last updated: November 2, 2025.