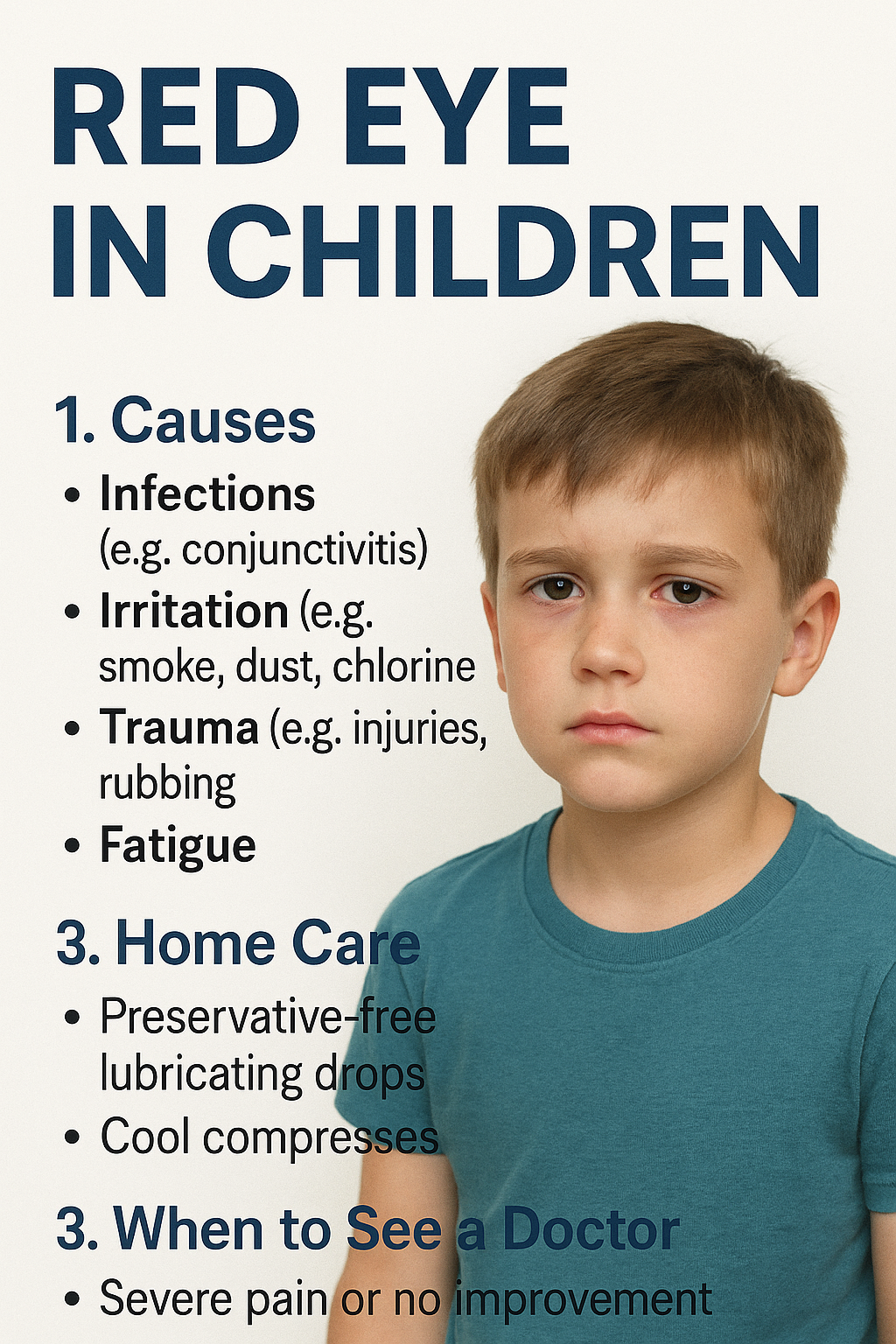
Red Eye in Children: Parent’s Guide to Causes, Home Care, and When to See a Doctor
Published: August 16, 2025
1. What Parents Should Know
Red eye in children happens when the tiny blood vessels on the eye’s surface swell from irritation, infection, or injury. Many cases are mild and short-lived, but some signal conditions that need prompt medical care. This guide explains the most common causes, safe home treatments, and clear warning signs so you’ll know exactly what to do.
2. Common Causes of Red Eye in Children
2.1 Conjunctivitis (Pink Eye)
- Viral: Often follows a cold; watery discharge; very contagious.
- Bacterial: Thicker yellow/green discharge and eyelid crusting; may need antibiotic drops.
- Allergic: Itchy, watery eyes with sneezing/runny nose; often seasonal or triggered by pets/dust.
2.2 Eye Irritation
- Exposure to smoke, chlorine from pools, strong wind, or dust.
- Small particles (sand, glitter) or soaps/shampoos that briefly contact the eye.
2.3 Trauma
- Accidental scratches from fingernails or toys.
- Sports injuries or blunt impact around the eye.
- Rubbing eyes vigorously, especially when already irritated or itchy.
2.4 Eye Strain or Fatigue
Prolonged screen time, reading in poor lighting, or not taking breaks can make eyes look red and tired.
2.5 More Serious Conditions (Less Common)
- Uveitis: Internal eye inflammation causing light sensitivity and ache—needs urgent evaluation.
- Acute glaucoma: Rare in kids, but redness with pain and vision changes is an emergency.
- Corneal abrasion/ulcer: From trauma or infection; often painful and light-sensitive.
3. Symptoms Parents Should Watch For
These clues help you decide between home care and medical assessment:
- Degree of redness and whether one or both eyes are involved.
- Type of discharge: watery vs. thick/yellow-green crusting.
- Itchiness (common in allergies) vs. pain/light sensitivity (more concerning).
- Vision changes, headache, or fever.
- Eyelid swelling or trouble opening the eye in bright light.
4. Home Care for Mild Cases
For mild redness from irritation, dryness, or tired eyes, try these parent-approved steps:
- Preservative-free lubricating eye drops (OTC): Start with one drop every hour for the first few hours, then reduce to 3–4 times daily as symptoms improve.
- Cool compress: Apply a clean, cool, damp cloth over closed lids for 5–10 minutes to soothe discomfort.
- Screen breaks: Encourage the 20-20-20 rule (every 20 minutes, look 20 feet away for 20 seconds).
- Hands off: Remind kids not to rub; trim nails and use tissues for gentle dabbing if needed.
- Allergy support: Keep windows closed on high-pollen days, rinse face after outdoor play, and wash bedding weekly in hot water.
Note: Avoid “redness-relief” vasoconstrictor drops in children unless your eye doctor recommends them; they can cause rebound redness.
5. Medical Treatments Your Doctor May Use
- Antibiotic drops/ointment: For bacterial conjunctivitis.
- Antihistamine/mast-cell stabilizer drops: For allergic conjunctivitis and itchy, watery eyes.
- Anti-inflammatory drops: For uveitis or significant inflammation (specialist guided).
- Corneal care: Pain control, protective shield, or bandage lens for abrasions; targeted therapy for ulcers.
6. Prevention Tips for Families
- Teach proper handwashing; provide personal towels and avoid sharing eye cosmetics.
- Use well-fitting sports goggles for ball sports and activities with flying debris.
- Limit chlorine exposure; rinse eyes with clean water after swimming and use swim goggles.
- Create balanced screen habits and encourage outdoor play for overall eye comfort.
- Manage allergies: air purifiers, dust-mite covers, and pet-free bedrooms when possible.
7. When to Seek Urgent Care
Contact your pediatrician or eye doctor right away if your child has:
- Severe pain, marked light sensitivity, or sudden vision changes.
- Thick discharge with fever or worsening redness/swelling.
- History of eye injury, a suspected foreign body, or chemical splash.
- Symptoms not improving within 24–48 hours of home care, or if both eyes become affected rapidly.
Conclusion
Most cases of red eye in children are mild and respond well to preservative-free lubricating drops, cool compresses, and screen breaks. Because redness can also signal infection or injury—especially after trauma—parents should watch for pain, light sensitivity, or vision changes and seek prompt care when these appear. With informed home care and timely medical guidance, you can protect your child’s comfort, vision, and eye health.