Diabetes and Eyesight
Diabetes Mellitis causes damage to all the blood vessels in the body, especially when it is poorly controlled. The blood vessels in the eye can be severely affected, leading to a loss of vision. Diabetes is one of the main causes of blindness in North Americans more than 40 years old.
Diabetes primarily affects the retina at the back of the eye, causing a disease called diabetic retinopathy. The retina’s blood vessels are damaged by diabetes. There are various stages of retinopathy.
The longer a person has diabetes, the greater the risk of eye disease. Type 1 diabetes, in which the body is not producing enough insulin, comes on earlier and can cause much higher blood sugars than type 2 diabetes. Patients are treated with insulin. 25% of patients with type 1 diabetes have retinopathy in 5 years; 80% have retinopathy after 15 years.
Type 2 diabetes occurs in part because parts of the body become resistant to insulin. There may also be a relative lack of insulin produced. This kind of diabetes can be treated with diet and exercise but frequently oral medications must be added. Insulin is not ordinarily needed. 25% of people who have had type 2 diabetes for 25 years or more develop proliferative diabetic retinopathy.
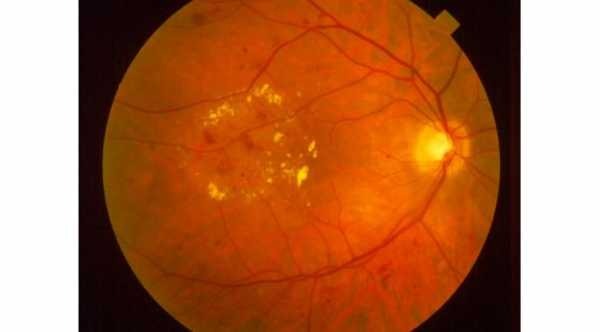
Non-proliferative retinopathy is the first stage. There are retinal abnormalities a doctor can see when examining the retina of a diabetic at this stage. There are changes in the blood vessels of the retina, including small areas of bleeding. There can be swelling of the retina and especially the macula, the part of the retina responsible for clear central vision. Deposits of fats can be seen. Damage to the blood vessels continues, and there are areas where not enough blood reaches the retina.
Eventually, new blood vessels will grow to try and supply blood to the retina. This is called proliferative retinopathy, when abnormal new blood vessels grow. These vessels can leak fluid or blood, further damaging vision. The new vessels can scar and cause traction on the retina which can cause tears in the retina.
There is an area of gel-like substance called the vitreous humor, between the iris/lens in front and the retina in back. With diabetic retinopathy, bleeding can occur into this area, causing loss of vision. Pressure in this area from swelling and bleeding can also cause the retina to detach from the back of the eye.
The new blood vessels can even grow into the front of the eye. This abnormal blood vessels are called iris rubeosis, causing glaucoma which is called neovascular glaucoma. So in addition to retinopathy, diabetics can develop glaucoma, which can be treated with drops, lasers, or surgery if needed.
At these advanced stages, permanent visual loss can occur from any or all of the abnormalities.
Also, elevated blood sugar affects the lens. If a diabetic’s blood sugar is going up and down a lot, the lens can swell and temporarily affect vision. Before buying new glasses, diabetics need their blood sugars need to be under control.
A more permanent lens problem is the formation of cataracts. These changes occur when the lens becomes clouded. Cataracts can occur earlier in diabetics than in people without diabetes. If they interfere with vision they can be removed and an artificial lens implanted. Read more about Symptoms of Diabetic Retinopathy.
Diabetic Retinopathy Treatment
All diabetics need regular eye examinations. These exams must be done with the pupil dilated so that the doctor can see the entire retina in the back of the eye. All diabetics need this done once a year. If they have developed diabetic retinopathy, they must be seen more frequently for evaluation and treatment.
Laser treatments are very good at preventing progression and visual loss. If there is just swelling of the macula, the laser will be focused there. If there is proliferative retinopathy, the entire retina will be treated. Sometimes removal of the vitreous body is helpful in a surgery called vitrectomy. An eye doctor can determine when this type of treatment is necessary and the most beneficial.
Much of the research in this area is focused on some medicines that may help treat diabetic retinopathy when injected into the back of the eye. These medicine are Anti-VEGF.
Tight control of blood sugar can help prevent diabetic retinopathy from beginning, as well as prevent existing retinopathy from getting worse. This has been proven by a number of large scientific studies. Controlling other medical problems, like high blood pressure, can also help prevent retinopathy from worsening.
Additionally, diabetics who have low vision can be given much need assistance by low vision specialists.
If you have diabetes and your doctor has not sent you to an ophthalmologist, you should ask to see one. If you can control your diabetes and follow the advice of the eye doctor regarding treatment, your vision can likely be saved.
Prevention of Diabetic Retinopathy
The best prevention of serious eye problems in diabetics is tight control of blood sugar. This is easier to do with young people who are diabetic.
Older diabetics are more likely to have episodes of excessively low blood sugar when trying to keep their blood sugar in the normal range. The best control possible should be the goal.
Other problems that diabetics can have, such as high blood pressure, add to the risk of diabetic eye disease, and should also be treated.